
Trigger Point Injection and Dry Needling
Precision Muscle Pain Relief for TMD, Headaches, and Myofascial Pain
Trigger points are tight, hyperirritable knots in muscles that can cause localized pain or refer pain to other areas of the head, neck, or jaw. These trigger points are frequently associated with myofascial pain, TMJ disorders, tension-type headaches, and facial pain syndromes. At Advanced TMJ Maxillofacial Pain & Sleep Center, we offer two highly effective treatments to deactivate these trigger points: Trigger Point Injections (TPI) and Dry Needling.
What Are Trigger Points?
Trigger points develop due to muscle overuse, stress, trauma, or postural imbalances. They are often found in the masseter, temporalis, sternocleidomastoid (SCM), and cervical muscles in patients with orofacial pain. These points can cause pain, restricted motion, muscle fatigue, and referred symptoms such as headaches or jaw discomfort.
What are Trigger Point Injections (TPI)?
Trigger point injections involve the precise insertion of a very fine needle into the trigger point, often followed by the injection of a small amount of local anesthetic (e.g., lidocaine) to relax the muscle and interrupt the pain cycle.
Evidence-Based Benefits:
-
Rapid reduction of muscle pain and tenderness
-
Improved range of motion and function
-
Reduced referred pain and headache frequency
-
Often used as part of a multimodal approach in managing myofascial TMD, chronic headaches, and facial pain
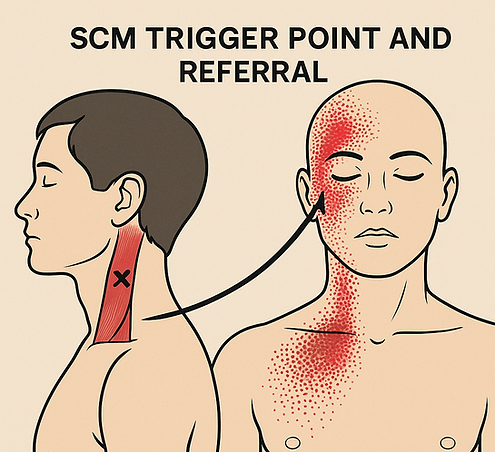
One of the most common muscle for developing Trigger points in the head and neck region is the Sternocleidomastoid (SCM).
The image here is a AI-generated pictorial representation of the likely areas where trigger points in SCM muscle can refer pain to.
It is not uncommon for patients suffering from TMJ disorders to have active SCM as the likely root cause for the pain.
For more information check this website for the full list of muscles and their associated trigger points. http://www.triggerpoints.net/
What is Dry Needling?
Dry needling uses the same fine needles as acupuncture but is rooted in Western anatomical science. No medication is injected. Instead, the mechanical action of the needle disrupts dysfunctional muscle fibers and stimulates a healing response.
How It Works:
-
Mechanical disruption of the trigger point
-
Increases blood flow and reduces local muscle spasm
-
Modulates pain signaling pathways through neuromuscular effects
Clinical Relevance:
Dry needling has shown promising outcomes in orofacial pain management. It is especially helpful for patients with myofascial pain, jaw clenching, tension-type headaches, and persistent postural-related muscle pain.
Research Insight:
Studies from the Journal of Bodywork and Movement Therapies and Pain Medicine suggest that dry needling provides significant pain relief, particularly when used alongside stretching, posture correction, or oral appliance therapy.
When Are These Treatments Recommended?
You may benefit from trigger point injections or dry needling if you have:
-
Persistent jaw or facial muscle pain
-
Recurrent headaches
-
Chronic TMJ pain unresponsive to conservative therapies
-
Limited jaw opening or neck mobility
-
A diagnosis of chronic facial pain or atypical facial pain
Why We Often Recommend Trigger Point Injections First?
-
Addresses the root cause: TPI breaks the pain cycle at its source — tight, painful muscle knots — rather than just masking symptoms.
-
Supports rehabilitation: Muscle function improves quickly, allowing you to start jaw stretches, posture correction, and physical therapy sooner.
-
Safe and reversible: No long-term paralysis or side effects. It's often diagnostic too — if you respond, it confirms myofascial pain as the cause.
Common Muscles Targeted in Trigger Point Injections/ Dry Needling for TMD & Orofacial Pain
-
Masticatory Muscles
-
Masseter
-
Most commonly injected
-
Pain refers to jaw, ear, teeth, and temple
-
-
Temporalis
-
Involved in clenching/grinding
-
Refers pain to the temples and supraorbital area
-
-
Medial Pterygoid
-
Refers pain to throat, TMJ, and inside the mouth
-
Accessed intraorally or transcutaneously (expert level)
-
-
Lateral Pterygoid
-
Deep muscle, rarely injected directly
-
Involved in disc displacement and jaw deviation
-
-
Cervical and Postural Muscles
-
Sternocleidomastoid (SCM)
-
Refers pain to jaw, around the eye, and vertex
-
-
Trapezius (Upper fibers)
-
Refers to occiput, jaw angle, and temporal region
-
-
Levator Scapulae
-
Can contribute to referred neck, TMJ and shoulder pain
-
-
Splenius Capitis / Cervicis
-
Refers to vertex, occiput, and temporal area
-
-
Other Head and Facial Muscles
-
Occipitalis
-
Related to tension headaches and scalp tenderness
-
-
Digastric (especially posterior belly)
-
Referred pain to throat, hyoid, and submandibular region
-
-
Mylohyoid & Geniohyoid
-
Contribute to oropharyngeal or submental pain patterns
-
-
Others as case basis
Why Choose Us?
At Advanced TMJ Maxillofacial Pain & Sleep Center, our board-certified Orofacial Pain specialist and Oral Surgeon is extensively trained in head and neck trigger point diagnostics and needling techniques, ensuring precision, safety, and evidence-based care. Every treatment is customized and often combined with complementary therapies like oral appliances, photobiomodulation, or neuromodulators for enhanced relief.








